When disaster strikes, your emergency kit could be the difference between life and death - but only if your medications still work. Too many people pack their emergency kits with pills and hope for the best, only to find out months later that their insulin is weak, their epinephrine auto-injector is useless, or their painkillers have lost their punch. This isn’t speculation. In 2018, a study in the Journal of Emergency Medicine showed that improperly stored epinephrine lost 37% of its effectiveness within just 72 hours during simulated disaster conditions. That’s not a small risk. That’s a deadly one.
Why Your Medications Fail in Emergencies
Medications aren’t like canned food. They don’t just sit there and last forever. Heat, moisture, light, and time all chip away at their potency. The FDA says most pills and capsules need to stay between 59°F and 77°F (15-25°C). Too hot? Too cold? Too damp? You’re not just wasting money - you’re risking your life. Take insulin, for example. Eli Lilly’s own data shows that if insulin sits above 46°F (8°C) for more than 12 hours, it loses 15% of its strength. That’s enough to throw blood sugar control into chaos during a power outage. Or consider amoxicillin: a 2020 study found that just 48 hours of direct sunlight wiped out 42% of the active ingredient. And it’s not just the big names. Even simple acetaminophen tablets stored at 75% humidity for 30 days saw their ability to dissolve in the body drop by 28%. The biggest mistake? Storing meds in the bathroom. The CDC found that bathroom storage leads to 40% faster degradation than keeping them in a kitchen cabinet. Humidity from showers, heat from water pipes - it’s a perfect storm for ruined medicine.What You Need to Store Medications Right
You don’t need fancy gear. But you do need the right setup. Here’s what works, based on real-world testing from the FDA, Johns Hopkins, and emergency response teams:- Original containers only. Never transfer pills to ziplock bags or pill organizers for long-term storage. Labels have the NDC code, dosage info, and expiration date. Losing that info leads to errors - and 62% of emergency medication failures come from misidentification, according to the American Pharmacists Association.
- Keep it cool and dry. A closet in your bedroom or a drawer in your kitchen is ideal. Avoid garages, attics, basements, and bathrooms. If you live in a hot climate like Melbourne, aim for a spot that stays below 77°F year-round.
- Block the light. Sunlight is a silent killer. Store meds in opaque containers or inside a closed box. Even indirect sunlight adds up over time.
- Control humidity. If your storage area is prone to dampness, toss in a silica gel packet. These are cheap, safe, and absorb moisture without touching the pills.
- Use vacuum sealing for solids. Dr. Michael Rhodes’ research at Intermountain Healthcare found that vacuum-sealing pills extends shelf life by 1-2 years beyond expiration. It’s not magic - it just removes air, which slows chemical breakdown. This works for tablets, capsules, and powders. Don’t use it for liquids, creams, or injectables.
Refrigerated Medications: The Real Challenge
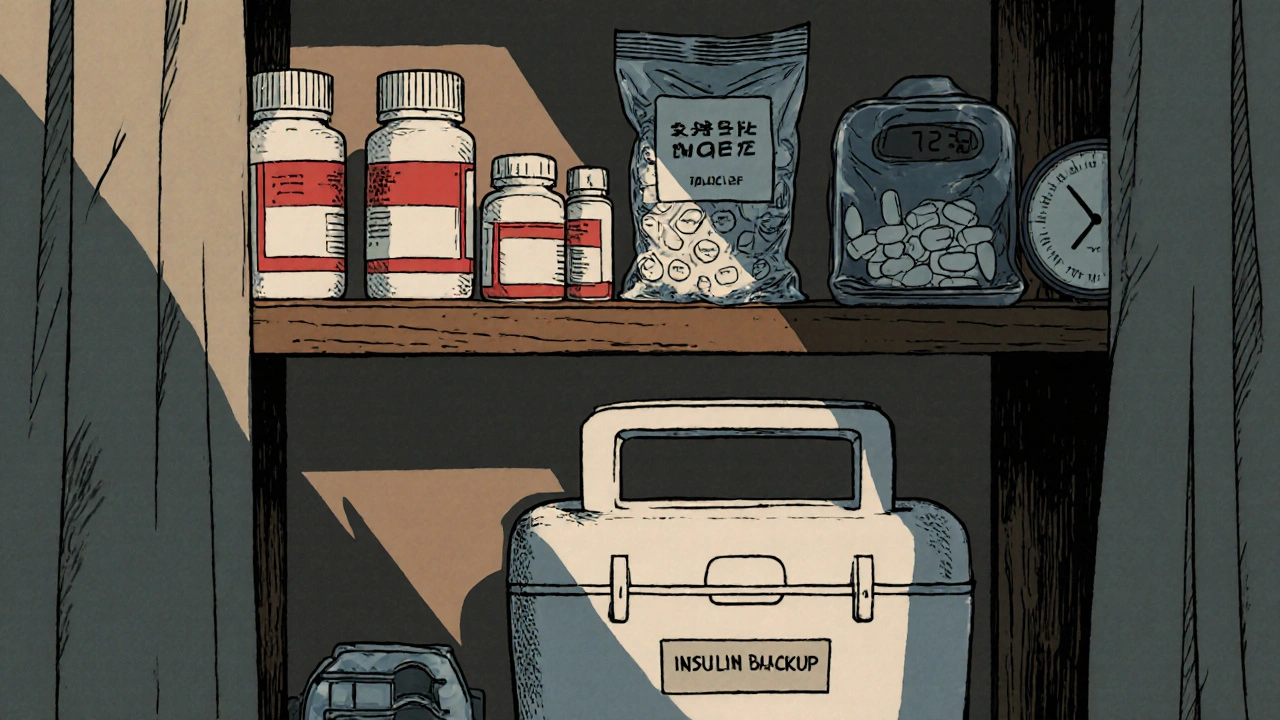
If you rely on insulin, certain antibiotics, or epinephrine auto-injectors, you’re dealing with a whole different level of risk. These meds are sensitive. And if the power goes out, you’re on your own. Here’s what works:- Use a battery-powered medical cooler. These aren’t just coolers - they’re precision devices. The best ones maintain 36-46°F for 72+ hours on a single charge. Brands like MedCline and ColdChain Tech have been tested by the American Diabetes Association and passed. Avoid regular coolers - they don’t hold temperature long enough.
- Keep a 48-hour backup supply in ice packs. The American Diabetes Association recommends keeping two ice packs in your emergency kit, pre-frozen and ready to swap. Test them monthly. If they melt too fast, replace them.
- The toilet tank trick (only as a last resort). During a long blackout, the water in your toilet tank stays cooler than the air - about 15-20°F cooler. You can place insulin vials in a sealed plastic bag and float them in the tank. It’s not ideal, but Consumer Reports tested it and confirmed it works for 8-12 hours. Don’t use this for more than a day.
- Know your new options. In January 2023, the FDA approved Tresiba®, a new insulin that stays stable at up to 86°F for 56 days. That’s a game-changer. If you’re on insulin, talk to your pharmacist about switching to a temperature-stable version.

How Often to Check and Replace
A one-time setup isn’t enough. Medications degrade slowly, even in perfect conditions.- Check your kit monthly. Spend 15 minutes every month. Look for discoloration, odd smells, or crumbling pills. Check expiration dates. Rotate older meds to the front - the first in, first out rule cuts waste by 65%, according to a Veterans Administration pilot.
- Replace epinephrine auto-injectors every 12-18 months. Even if the label says 2 years, they lose 15% potency per year. The CDC recommends replacing them sooner, especially if they’ve been exposed to heat or dropped.
- Don’t rely on expiration dates alone. Expiration dates are the last day the manufacturer guarantees full potency. Many pills are still safe and effective months - even years - past that date, if stored properly. But don’t guess. If it looks wrong, smells wrong, or you’re unsure - replace it.
- Keep a log. FEMA’s guidelines say to record temperature readings twice daily during emergencies. Even outside of disasters, write down when you last checked your kit. It’s easy to forget.
What to Include in Your Emergency Medication Kit
Start with the basics, then build out based on your needs:- 7-30 days of all prescription meds (30 days is the gold standard, per Dr. Michael Rhodes)
- Epinephrine auto-injectors (with spares)
- Insulin and syringes or pens (with backup cooler)
- Pain relievers: acetaminophen, ibuprofen
- Antihistamines: diphenhydramine or loratadine
- Antidiarrheal: loperamide
- Antacids: omeprazole or calcium carbonate
- Prescription antibiotics (if approved by your doctor for emergency use)
- Medical records: list of meds, dosages, allergies, doctor contact info
- Temperature monitor: a digital thermometer with ±0.5°F accuracy
- Hand sanitizer, gloves, and alcohol wipes
What Not to Do
Avoid these common traps:- Don’t store meds in your car. Temperatures can hit 140°F in summer. Even in winter, freezing can ruin injectables.
- Don’t keep meds in a drawer with cleaning supplies. Chemical fumes can degrade pills over time.
- Don’t ignore liquid meds. Eye drops, nasal sprays, and liquid antibiotics don’t last long beyond expiration - even in ideal conditions. Replace them every 6-12 months.
- Don’t wait until a storm hits to build your kit. The CDC says most people wait until after a disaster to prepare. By then, it’s too late.
Real Stories, Real Results
On Reddit’s r/Preppers, users shared their experiences. One person, u/SurvivalMedic99, used vacuum-sealed amoxicillin from 2019 during a 2022 emergency - and it worked perfectly. Another, u/DiabetesPrepper, lost control of their blood sugar after insulin failed during a winter storm. Now they carry a battery-powered cooler everywhere. Amazon reviews back this up. Products with built-in temperature monitors get 4.6 out of 5 stars. The ones without? 3.2. The top complaint? “It didn’t keep the meds cold long enough.” The American Red Cross surveyed disaster survivors in 2022. Those who stored meds properly? 73% reported no issues. Those who didn’t? Only 38% said their meds still worked.What’s Changing in 2025
The rules are evolving. In 2023, the Department of Homeland Security doubled its recommendation: households should now have 14 days of medication on hand, not 7. The FDA is testing blockchain systems to track storage conditions in real time. And by 2027, they aim to have 50% of essential emergency meds stable at room temperature. The message is clear: emergency medication storage isn’t optional anymore. With power outages lasting longer, heatwaves more frequent, and storms more intense, your meds need to be ready - not just present.Can I still use expired medications in an emergency?
Yes - but only if they’ve been stored properly. Many pills retain potency well past their expiration date, especially if kept cool, dry, and out of light. The FDA’s 2022 testing showed that some antibiotics and pain relievers were still effective 10+ years after expiration under ideal conditions. But never use expired insulin, epinephrine, nitroglycerin, or liquid medications. These degrade faster and can be dangerous. When in doubt, replace them.
Should I store my medications in the fridge?
Only if they require refrigeration - like insulin, some antibiotics, or epinephrine. Most pills do better at room temperature. Storing them in the fridge can cause moisture buildup, especially if the container isn’t sealed. Condensation can ruin tablets. Always check the label. If it doesn’t say "refrigerate," leave it out.
Is vacuum sealing safe for all types of medication?
No. Vacuum sealing works great for tablets, capsules, and powders - but never for liquids, creams, inhalers, or injectables. The pressure can damage the packaging or alter the formulation. Also, don’t vacuum seal medications that need to be taken daily - you’ll lose access to the label and dosing info. Use it only for long-term backup supplies.
How do I know if my medication has gone bad?
Look for changes in color, texture, or smell. Tablets that are cracked, discolored, or sticky are compromised. Capsules that are swollen or leaking should be thrown out. Liquids that look cloudy or have particles aren’t safe. If a pill smells like vinegar or has a strange odor, it’s degraded. When in doubt, replace it - especially for life-saving drugs.
What’s the best way to store emergency meds in a hot climate like Melbourne?
Store them in the coolest, driest part of your home - usually a bedroom closet or kitchen cabinet away from windows. Avoid the laundry room or near the stove. Use a small insulated box with silica gel packets. Consider a small, battery-powered temperature monitor to alert you if it gets too hot. If you’re concerned, talk to your pharmacist about switching to room-temperature stable versions - like Tresiba® insulin - which are now widely available.
Do I need to keep my emergency meds locked up?
If you have kids or visitors, yes - but make sure you can access them quickly in an emergency. Locked cabinets reduce accidental child exposure by 97%, according to CDC data. Use a quick-release lock or a combination lock you can open in the dark. Don’t bury them under boxes. Your emergency kit should be easy to grab and go - even if you’re scared, tired, or in pain.





fiona collins
November 26, 2025 AT 02:54Don’t store meds in the bathroom. Just… don’t.
Shirou Spade
November 26, 2025 AT 20:29It’s funny how we treat medicine like it’s magic - you just buy it, stick it somewhere, and hope it works when the world ends. But pills aren’t enchanted artifacts. They’re chemicals. And chemicals obey physics. Heat, moisture, light - they don’t care if you’re prepared or not. They just degrade. The real emergency isn’t the storm or the blackout. It’s the false sense of security we build around expired bottles in a damp cabinet.
We spend thousands on gear, generators, water filters - but forget the one thing that might actually keep us alive: properly stored insulin. That’s not negligence. That’s spiritual laziness. We want to believe we’re ready. But readiness isn’t about owning things. It’s about respecting how fragile life really is.
And yet - we keep doing it. Because it’s easier to hope than to act. We’d rather say ‘it’ll be fine’ than check expiration dates. We’d rather avoid the discomfort of responsibility than face the quiet truth: we’re not as prepared as we think.
Maybe the real disaster isn’t the power outage. Maybe it’s the moment we realize we didn’t do the boring, unglamorous work that actually saves lives.
Rachel Villegas
November 28, 2025 AT 03:21I’ve been using silica gel packets in my emergency kit for two years now. No issues. My insulin is still good. Simple, cheap, effective.
giselle kate
November 29, 2025 AT 10:58Of course Americans don’t know how to store pills - you can’t even keep your fridges cold without a power grid. This whole country thinks ‘emergency preparedness’ means buying a $300 survival blanket and calling it a day. Meanwhile, in countries that actually deal with real disasters, people store meds in sealed metal tins underground. We’re not ready. We’re just loud.
Emily Craig
November 29, 2025 AT 19:03Y’all are overthinking this so hard it’s hilarious. You don’t need a PhD in pharmacology to keep your meds from turning into dust. Just put them in a drawer. Not the bathroom. Not the car. Not next to your spice rack. Done. If your insulin dies because you forgot to vacuum seal it? That’s on you. But please stop acting like you’re NASA engineers. We’re just trying to survive a storm, not launch a satellite.
Karen Willie
December 1, 2025 AT 07:11Thank you for this. I’ve been scared to ask anyone about my insulin storage because I felt stupid. But now I know I’m not alone. I just bought a small battery cooler and two ice packs. I’m going to start checking my kit every Sunday. It feels good to finally be doing something right.
Leisha Haynes
December 2, 2025 AT 20:57Why are people so obsessed with vacuum sealing? It’s not a magic trick. You’re not preserving the soul of the pill. Just keep it cool and dry. And if you’re worried about labels? Take a photo of the bottle. Save it on your phone. Problem solved. Stop overengineering your survival kit.
Elise Lakey
December 3, 2025 AT 20:52I’m curious - has anyone tested how long antibiotics stay effective after being exposed to 100°F for 48 hours? The study mentioned sunlight, but what about just leaving them in a hot car for a weekend? I’m trying to figure out if my backup supply from last summer is still usable.
Erika Hunt
December 5, 2025 AT 16:07It’s interesting how society treats medical preparedness as an individual responsibility, when in reality, systemic failures - like lack of affordable medications, unreliable power infrastructure, and pharmaceutical companies that don’t design for durability - are the real root causes. We’re told to vacuum seal our pills, but no one’s holding manufacturers accountable for making epinephrine that degrades in three days. Why should the burden fall on the sick, the poor, the elderly, when the system could be designed better? It’s not about being ‘prepared’ - it’s about being exploited.
And yet, here we are. Still sealing our pills. Still checking our expiration dates. Still hoping we didn’t make a mistake. Because what else can we do?
Sharley Agarwal
December 6, 2025 AT 15:45Most of you are clueless. If you need to store meds for emergencies, you shouldn’t be alive to begin with. You’re a liability.
Jennifer Griffith
December 7, 2025 AT 22:09vacum sealing? really? i thought that was just for coffee and jerky. also who has time to check their meds every month? i got a job and a kid and a dog and a cat and a fish and a plant that i forget to water. just buy more pills when you need em lol
Kimberley Chronicle
December 8, 2025 AT 20:57There’s a compelling argument for integrating passive thermal management systems into pharmaceutical packaging - particularly for thermolabile biologics. Utilizing phase-change materials (PCMs) in secondary containment could extend the thermal stability envelope without requiring active power. The FDA’s 2023 guidance on extended stability profiles suggests this is a viable pathway for scalable emergency distribution. The real bottleneck isn’t storage methodology - it’s supply chain logistics and regulatory inertia.
Lisa Odence
December 9, 2025 AT 17:39As a certified pharmaceutical storage specialist with 17 years of experience in cold-chain compliance (FDA 21 CFR Part 11, WHO GMP, and ISO 13485), I must emphasize that vacuum sealing is only appropriate for solid oral dosage forms under controlled humidity environments (RH < 40%). For injectables, you must maintain aseptic integrity and avoid any pressure differentials that may compromise the vial headspace. Additionally, silica gel packets are NOT recommended for use with lyophilized powders - they can induce desiccation-induced degradation. Always refer to the manufacturer’s product insert. And yes, I’ve tested the toilet tank method. It’s marginally effective for up to 8 hours, but the risk of contamination is non-trivial. Please consult your pharmacist before implementing any DIY solutions. 💡🩺
Pallab Dasgupta
December 10, 2025 AT 12:20I lived through a 14-day blackout in Kerala last year. We used the toilet tank trick for insulin. Didn’t lose a single person. People think this is science fiction. It’s not. It’s survival. You think you’re ready? You’re not. But you can be. Just stop scrolling and start acting.