Gonorrhea Symptom Checker
Symptom Assessment
This tool helps you understand potential symptoms of gonorrhea that affect cervical health. Answer the following questions honestly to get personalized feedback.
Your symptom assessment will appear here. Click "Check My Risk Level" to see personalized feedback based on your responses.
Understanding Gonorrhea and its impact on cervical health is crucial for women who want to stay in control of their wellbeing. This guide explains how the infection works, why the cervix matters, how to spot warning signs, and what steps protect you from long‑term complications.
What is Gonorrhea?
Gonorrhea is a bacterial sexually transmitted infection caused by Neisseria gonorrhoeae. In the United States, the CDC reports over 600,000 new cases each year, with women accounting for roughly 30% of infections. The bacterium thrives in warm, moist mucous membranes, making the cervix a prime site for colonisation.
Why Cervical Health Matters
The cervix is the gateway between the vagina and uterus, lined with delicate cells that can become inflamed or damaged when exposed to infections. Persistent inflammation can lead to scarring, disrupted menstrual flow, and, in rare cases, increase the risk of cervical cancer when combined with other high‑risk infections such as human papillomavirus (HPV).
Cervix is the lower part of the uterus that opens into the vagina and plays a key role in fertility and menstrual health. Keeping it healthy means regular screenings, safe sex practices, and prompt treatment of any STI.
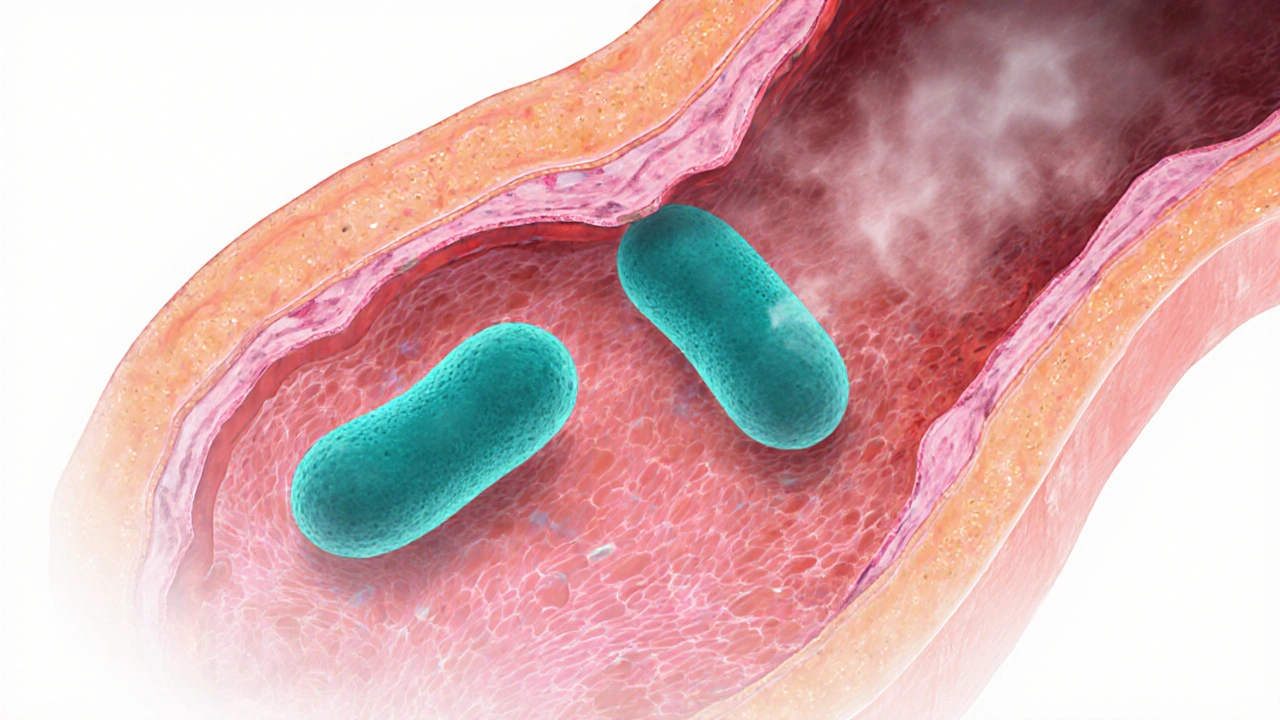
How Gonorrhea Affects the Cervix
- Direct infection of cervical cells can cause cervicitis, characterized by painful bleeding, discharge, and swelling.
- Inflammation may make the cervical tissue more susceptible to HPV infection, which is the leading cause of cervical cancer.
- Untreated gonorrhea can ascend to the uterus, fallopian tubes, and surrounding organs, potentially triggering pelvic inflammatory disease (PID).
Pelvic inflammatory disease is an infection of the female reproductive organs that can cause chronic pelvic pain and infertility often results from delayed treatment of gonorrhea or chlamydia.

Common Symptoms in Women
Many women experience mild or no symptoms, which is why regular testing is essential. When symptoms do appear, they often include:
- Thin, watery vaginal discharge that may be clear or slightly yellow.
- Burning sensation during urination.
- Bleeding between periods or after intercourse.
- Lower abdominal or pelvic pain.
These signs overlap with other STIs, especially Chlamydia a bacterial infection that frequently co‑occurs with gonorrhea and shares similar symptoms. Because the presentations are so alike, a single laboratory test can identify both pathogens.
Testing and Diagnosis
The most reliable method is nucleic acid amplification testing (NAAT), which detects bacterial DNA from a urine sample or a swab taken from the cervix. NAATs have a sensitivity above 95% and can simultaneously screen for gonorrhea, chlamydia, and sometimes even trichomoniasis.
For women who prefer a self‑collection option, the CDC endorses at‑home kits that ship a swab to a certified lab. Results are typically available within 3-5 days, and a telemedicine visit can be arranged for prescribing treatment.
Treatment Options and Antibiotic Resistance
Current guidelines recommend a dual‑therapy approach: a single intramuscular injection of ceftriaxone (250mg) plus oral azithromycin (1g) to cover potential co‑infection. This regimen remains effective for most strains, but rising antibiotic resistance is a growing concern worldwide.
Antibiotic resistance refers to the ability of bacteria like Neisseria gonorrhoeae to survive drugs that previously killed them has prompted the CDC to monitor resistant cases and update treatment protocols annually.
- If you have a known allergy to ceftriaxone, alternative regimens such as cefixime combined with doxycycline may be used under clinician supervision.
- Completing the full dose is critical; missing a dose can foster resistant strains and prolong infection.
Because resistant gonorrhea strains can spread quickly, prompt testing, full‑dose treatment, and notifying sexual partners are essential public‑health steps.

Preventive Measures for Women
Prevention is a blend of behavioural choices and medical safeguards:
- Consistent use of latex or polyurethane condoms reduces transmission risk by up to 80%.
- Limit the number of sexual partners and encourage regular STI screening for anyone who is sexually active.
- Consider HPV vaccination, which protects against the high‑risk strains that contribute to cervical cancer. Though it does not prevent gonorrhea, it lessens the compounded risk of co‑infection.
- Routine cervical screening (Pap smear or HPV test) every three years for women aged 21-29, and every five years for those 30-65 when combined with HPV testing, catches abnormal cell changes early.
Human papillomavirus is the most common sexually transmitted virus and a leading cause of cervical cancer vaccination programs have lowered cervical cancer rates dramatically, highlighting the power of prevention.
Comparing Gonorrhea and Chlamydia
| Feature | Gonorrhea | Chlamydia |
|---|---|---|
| Cause | Neisseria gonorrhoeae (bacterium) | Chlamydia trachomatis (bacterium) |
| Typical Symptoms in Women | Discharge, burning urination, bleeding after sex | Often asymptomatic; if present, similar discharge and pain |
| Preferred Test | NAAT (urine or cervical swab) | NAAT (urine or cervical swab) |
| Treatment | Ceftriaxone + Azithromycin | Doxycycline 100mg twice daily for 7days |
| Resistance Concerns | Increasing global ceftriaxone resistance | Low resistance; doxycycline remains effective |
Both infections share transmission routes and can coexist, which is why clinicians often treat them together until test results clarify the exact pathogen.
What to Do If You Test Positive
- Schedule a follow‑up appointment (in‑person or telehealth) to discuss treatment options.
- Take the prescribed antibiotics exactly as directed; do not skip doses.
- Inform current sexual partners so they can get tested and treated promptly.
- Abstain from vaginal intercourse until you and your partners have completed treatment and a 7‑day symptom‑free period has passed.
- Retest in 3 months to confirm the infection is cleared, especially if you have new or multiple partners.
Failing to complete these steps can lead to chronic cervicitis, PID, infertility, and higher susceptibility to other infections.
Frequently Asked Questions
Can gonorrhea cause cervical cancer?
Gonorrhea itself does not cause cervical cancer, but the inflammation it creates can make the cervix more vulnerable to high‑risk HPV infection, which is the direct cause of most cervical cancers.
Is a urine test enough to detect cervical infection?
Yes. Modern NAATs can detect gonorrhea DNA in a first‑catch urine sample with the same accuracy as a cervical swab. However, a swab may be preferred if your doctor wants to assess local cervical inflammation directly.
How soon after exposure should I get tested?
Testing is reliable about 5-7days after exposure. If you test earlier and receive a negative result, retest after one week to rule out a false‑negative.
Can I get pregnant while being treated for gonorrhea?
Pregnancy is possible, but the infection can harm the developing fetus and increase the risk of preterm birth. Discuss treatment timing with your healthcare provider if you are trying to conceive.
What are the signs of antibiotic‑resistant gonorrhea?
Persistent symptoms after a full course of recommended antibiotics signal possible resistance. Your doctor may order a culture and susceptibility test to select an alternative regimen.
Staying informed about gonorrhea, getting screened regularly, and acting quickly if an infection is found protects not only your cervix but your whole reproductive future.






Julia Odom
October 7, 2025 AT 14:19Thank you for this comprehensive overview; the articulation is both meticulous and vivid. Your distinction between the direct effects of gonorrhea on cervical tissue and the indirect risk of HPV co‑infection is especially illuminating. The inclusion of up‑to‑date statistics lends authority to the discussion, and the practical steps for prevention are articulated with clarity. Overall, this piece serves as an excellent educational resource for women seeking to safeguard their reproductive health.
Danielle Knox
October 13, 2025 AT 09:12Oh great, another lecture on why condoms are a good idea. As if we needed another reminder about basic hygiene. The table comparing gonorrhea and chlamydia is just a copy‑paste from the CDC brochure.
Mark Evans
October 19, 2025 AT 04:05I hear you, Danielle, but the data really does matter. When people skim over the differences, they miss the chance to get tested early, which can prevent PID. Sharing the simple urine‑test fact is a lifesaver for many who are nervous about pelvic exams. Let’s keep the focus on practical access, not just sarcasm.
Megan C.
October 24, 2025 AT 22:59Honestly, it’s disheartening to see anyone treat STIs as a casual topic. The moral responsibility to get tested and to inform partners cannot be overstated. Ignoring these guidelines contributes to a cycle of infection that disproportionately harms women. We must uphold a higher standard of care and accountability.
Greg McKinney
October 30, 2025 AT 16:52If you’re going to preach about responsibility, don’t forget that some people simply don’t have access to regular screenings. The system itself can be a barrier, so blaming individuals exclusively is a bit myopic.
Dawna Rand
November 5, 2025 AT 11:45👍 Great job laying out the facts! 🌟 It’s so important to remember that a quick test can save you from a lot of stress later. Keep spreading the word and don’t forget to schedule those regular check‑ups! 💪
Effie Chen
November 11, 2025 AT 06:39Thanks for the clear guide 🙏. I’m curious about the timeline for resistance testing-how often should labs re‑check the strain’s susceptibility after treatment? 🤔
rohit kulkarni
November 17, 2025 AT 01:32Allow me to expand upon the intricate interplay between Neisseria gonorrhoeae and the cervical epithelium; the bacterium, when it adheres to the columnar cells of the endocervix, initiates a cascade of inflammatory mediators that, in turn, compromise the mucosal barrier. This disruption is not merely a fleeting irritation-it precipitates a microenvironment conducive to secondary viral colonisation, most notably oncogenic strains of human papillomavirus. The literature, from seminal works in the 1990s to recent genomic analyses, consistently demonstrates that persistent cervicitis augments the likelihood of integration of HPV DNA into host chromosomes, thereby escalating oncogenic risk. Moreover, the pathogen’s capacity for antigenic variation, mediated by pilus phase‑variation and outer membrane protein remodeling, enables it to evade innate immune detection, prolonging infection and exacerbating tissue damage. Antibiotic resistance, a burgeoning crisis, compounds these issues: as the efficacy of ceftriaxone wanes, clinicians are compelled to resort to alternative regimens that may possess inferior tissue penetration, further compromising eradication. The sociocultural dimension cannot be ignored-stigma surrounding STI testing frequently delays presentation, permitting the infection to ascend to the uterine cavity and fallopian tubes, culminating in pelvic inflammatory disease. PID, in turn, is the principal antecedent of tubal factor infertility, a tragic outcome that could have been prevented with timely screening. From a public‑health perspective, the implementation of point‑of‑care nucleic acid amplification tests has demonstrated a reduction in diagnostic latency, yet accessibility remains uneven across socioeconomic strata. Consequently, targeted outreach programs and subsidized testing kits are indispensable. In summation, the confluence of bacterial pathogenicity, host immune response, antimicrobial resistance, and systemic barriers coalesce to render gonorrhea a formidable adversary to cervical health; vigilance, rapid diagnostics, and comprehensive treatment protocols are the pillars upon which we must build our defense.
RONEY AHAMED
November 22, 2025 AT 20:25Nice work, the checklist format really helps people see what to watch for. Just remember that a single symptom doesn’t always mean infection.
emma but call me ulfi
November 28, 2025 AT 15:19Appreciate the low‑key tone-makes the info less scary. I’ll definitely keep the reminder about retesting in a few months.
George Gritzalas
December 4, 2025 AT 10:12Wow, who wrote this? Someone clearly loves commas-so many of them! Anyway, the content is solid, just wish the formatting wasn’t a drama fest.
Alyssa Matarum
December 10, 2025 AT 05:05Good read.
Lydia Conier
December 15, 2025 AT 23:59Thanks for the thorough guide! I really love the emoji‑friendly layout-makes it feel less like a textbook and more like a friend chatting. One tiny thing: I noticed a few typos (like “cervix is the lower part” should be “cervix is the lower …”) but honestly that doesn’t take away from the solid info. Keep it up!
ruth purizaca
December 21, 2025 AT 18:52Honestly, the article could have cut the fluff and just stuck to the facts-you know, the quick bullet points.
Shelley Beneteau
December 27, 2025 AT 13:45I’m intrigued by the recommendation to combine HPV vaccination with regular STI screening. It seems a holistic approach that could really shift public‑health outcomes if adopted widely.
Sonya Postnikova
January 2, 2026 AT 08:39What an empowering piece! 🌈 Remember, knowledge is power-so let’s share this with everyone we care about. 👭
Anna Zawierucha
January 8, 2026 AT 03:32Sure, gonorrhea is “just another STI,” but hey, at least it doesn’t come with a free Netflix subscription.
Mary Akerstrom
January 13, 2026 AT 22:25Great job keeping it clear and helpful thanks for sharing