Choosing the right drug for Parkinson’s tremor or drug‑induced movement disorders can feel like navigating a maze. You want relief without a laundry list of side effects, and you often hear the name Artane tossed around. But is it truly the best fit for you or your loved one? This guide breaks down Artane (trihexyphenidyl) side‑by‑side with its most common rivals, so you can see the trade‑offs at a glance and talk to your doctor with confidence.
What is Artane (Trihexyphenidyl)?
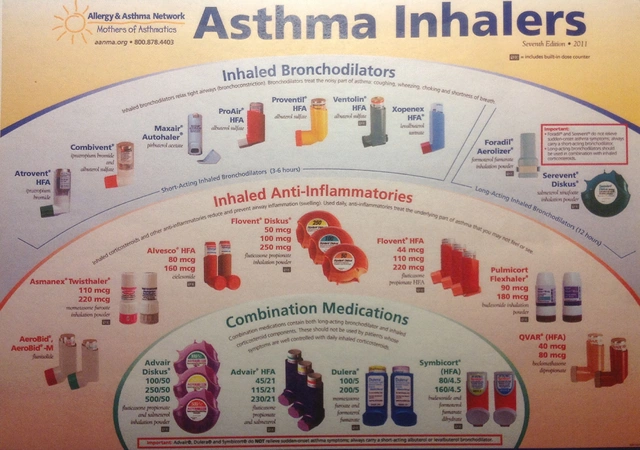
Artane (Trihexyphenidyl) is an anticholinergic medication used primarily to treat Parkinson’s disease‑related tremor and extrapyramidal side effects caused by neuroleptic drugs. It works by blocking acetylcholine receptors in the brain, helping to rebalance dopamine‑acetylcholine signaling that becomes skewed in Parkinson’s.
Typical dosing for adults starts at 0.5‑2 mg daily, titrated up to 10‑15 mg in divided doses depending on response and tolerance. Because it crosses the blood‑brain barrier, it’s effective for motor symptoms but can also affect the central nervous system, leading to a distinct side‑effect profile.
Key Factors to Weigh When Comparing Anticholinergic Drugs
- Mechanism of action: All anticholinergics share the same basic pathway, but potency and receptor selectivity differ.
- Age considerations: Younger patients (<65) tend to tolerate anticholinergics better; older adults face higher risks of cognitive decline.
- Side‑effect burden: Dry mouth, constipation, blurred vision, and especially central effects like memory loss or confusion.
- Drug interactions: Concurrent use with antihistamines, tricyclic antidepressants, or other anticholinergics can amplify adverse effects.
- Clinical goals: Is tremor the main issue, or are rigidity and bradykinesia more prominent? Some alternatives target a broader symptom set.
Major Alternatives to Artane
While Artane remains a go‑to for tremor‑dominant Parkinson’s, several other agents are frequently prescribed. Below are the most widely used:
Benztropine (Cogentin)
Benztropine is another anticholinergic, often favored because it has a slightly shorter half‑life and may cause fewer cognitive side effects in younger patients. Doses range from 0.5 mg daily up to 6 mg per day in divided doses.
Biperiden (Akineton)
Biperiden offers a middle ground-strong anticholinergic effect with a lower incidence of dry mouth compared to Artane. Typical dosing is 1‑2 mg two to three times daily, max 12 mg per day.
Amantadine
Amantadine isn’t an anticholinergic; it works by releasing dopamine and blocking NMDA receptors. It can improve both tremor and mild dyskinesia, making it a popular adjunct. Starting dose is 100 mg once daily, often increased to 200 mg twice daily.
Levodopa & Dopamine Agonists
For patients whose symptoms extend beyond tremor, Levodopa (often combined with carbidopa) and dopamine agonists such as pramipexole or ropinirole become the backbone of therapy. These aren’t direct alternatives for anticholinergic‑only treatment but are worth mentioning when evaluating overall medication strategy.
Side‑Effect Profiles at a Glance
| Drug | Mechanism | Typical Dose | Common Side Effects | Best For | Not Ideal When |
|---|---|---|---|---|---|
| Artane (Trihexyphenidyl) | Anticholinergic | 0.5‑15 mg/day (divided) | Dry mouth, constipation, blurred vision, confusion, memory loss | Younger patients with tremor‑dominant PD | Patients >70 yr, pre‑existing cognitive issues |
| Benztropine | Anticholinergic | 0.5‑6 mg/day | Less dry mouth than Artane, but still constipation, urinary retention | Younger adults needing rapid tremor control | Elderly, severe glaucoma |
| Biperiden | Anticholinergic | 1‑12 mg/day | Dry mouth, mild dizziness, rare cognitive impact | Patients who can’t tolerate Artane’s dose‑related side effects | Renal impairment (requires dose adjustment) |
| Amantadine | Dopamine release/NMDA antagonism | 100‑200 mg 1‑2×/day | Leg swelling, livedo reticularis, insomnia | Patients with mild dyskinesia or combined tremor‑rigidity | Severe renal disease (dose cuts) |
Practical Guidance: Who Should Choose Artane?
- Younger age group (under 65): Cognitive side effects are less pronounced, making Artane a solid first‑line anticholinergic.
- Tremor‑dominant Parkinson’s: If rigidity and bradykinesia are mild, Artane can target tremor without the need for dopaminergic therapy.
- No history of glaucoma or urinary retention: Anticholinergics can worsen these conditions.
- Ability to adhere to multiple daily doses: Artane often requires split dosing for steady symptom control.
If any of the above don’t apply, you may want to discuss Benztropine, Biperiden, or even a non‑anticholinergic like Amantadine with your neurologist.
Switching or Combining Medications
- Gradual taper: When moving from Artane to another anticholinergic, reduce the dose by 25‑30% every 3‑5 days to avoid rebound tremor.
- Overlap period: A short 2‑week overlap can smooth the transition, especially if the new drug has a slower onset (e.g., Amantadine).
- Monitor for additive anticholinergic load: Never combine two anticholinergics at full doses; the risk of delirium rises sharply.
Checklist Before Deciding on an Anticholinergic
- Have you discussed all non‑pharmacologic options (exercise, physiotherapy)?
- Is tremor the primary disabling symptom?
- Do you have any history of cognitive impairment, glaucoma, or urinary blockage?
- Are you on other medications with anticholinergic properties?
- Can you commit to regular blood pressure and liver function monitoring?
Answering these questions with your clinician will narrow the field quickly.
Frequently Asked Questions
Can I take Artane together with Levodopa?
Yes, many patients use Artane alongside Levodopa to control tremor while Levodopa handles rigidity and bradykinesia. However, the combination can increase nausea, so dose adjustments may be needed.
Why do some doctors prefer Benztropine over Artane?
Benztropine has a shorter half‑life and tends to produce fewer central side effects in patients under 70 years. It also requires fewer dose adjustments for renal impairment.
Is Biperiden safe for elderly patients?
Biperiden can be used in older adults, but the dose should start low (1 mg once daily) and be increased slowly. Cognitive monitoring is essential because anticholinergic load remains a concern.
What should I do if I experience severe dry mouth?
Sip water frequently, chew sugar‑free gum, or ask your doctor about a saliva substitute. In some cases, the clinician may lower the anticholinergic dose or switch to a drug with less salivary impact.
Can I stop Artane abruptly?
Abrupt discontinuation can cause rebound tremor and agitation. Tapering over 1‑2 weeks is recommended, under medical supervision.
At the end of the day, the “best” drug is the one that balances symptom relief with tolerable side effects for your unique health picture. Use this comparison as a starting point, bring the table to your neurologist, and decide together which path feels right.






Latasha Becker
October 19, 2025 AT 21:28The pharmacodynamic profile of trihexyphenidyl is frequently oversimplified in patient education materials.
Its antagonism of muscarinic M1 receptors not only attenuates central cholinergic hyperactivity but also precipitates a cascade of downstream neurochemical adjustments.
Consequently, clinicians must evaluate the drug‑induced modulation of the striatal interneuron network rather than merely counting milligrams.
Empirical evidence from double‑blind trials indicates a dose‑response curve that plateaus beyond 8 mg daily for tremor suppression.
Above this threshold, the incidence of xerostomia, urinary retention, and cognitive slowing rises exponentially.
Moreover, the interindividual variability in blood‑brain barrier permeability renders plasma concentrations a poor surrogate for central efficacy.
Pharmacogenomic markers, such as CYP2D6 polymorphisms, have been correlated with altered metabolite ratios, thereby influencing both therapeutic window and adverse‑event profile.
When juxtaposing trihexyphenidyl with benztropine, the latter exhibits a shorter half‑life and a marginally superior side‑effect tolerability in patients under seventy.
Nevertheless, benztropine’s anticholinergic load is not negligible and may synergize with concomitant antihistamines to exacerbate delirium.
The clinician’s decision matrix should therefore incorporate age‑related blood‑brain barrier permeability, comorbid ocular hypertension, and polypharmacy burden.
In practice, a titration schedule commencing at 0.5 mg nightly and escalating by 0.5 mg weekly allows objective assessment of motor benefit versus neurocognitive trade‑off.
Objective scales such as the Unified Parkinson’s Disease Rating Scale (UPDRS) tremor subscore provide quantifiable endpoints for dose adjustment.
Patients presenting with isolated tremor may achieve comparable control with lower‑dose amantadine, which also offers neuroprotective glutamate antagonism.
However, the risk of peripheral edema and livedo reticularis with amantadine necessitates vigilant dermatologic monitoring.
In summary, trihexyphenidyl remains a viable first‑line anticholinergic for younger patients with tremor‑dominant Parkinsonism, provided that clinicians meticulously balance pharmacokinetic nuances with individual comorbidity profiles.
parth gajjar
October 19, 2025 AT 21:45Oh the tragedy of trembling hands the silent plea for a pill that promises calm yet the world of meds is a theater of shadows where each dose conjures its own ghosts the bitter taste of dry mouth feels like a desert inside the mouth while the mind spins in a fog the drama of dosage titration becomes a ballet of hope and despair each night the mirror reflects a battle between tremor and side effects
Maridel Frey
October 19, 2025 AT 22:01For anyone navigating the complexities of anticholinergic therapy, it is essential to first map out the individual’s comorbid conditions, cognitive baseline, and daily routine. A structured checklist, similar to the one outlined in the article, can serve as a decision‑making scaffold. When introducing trihexyphenidyl, start at the lowest feasible dose and schedule follow‑up assessments at two‑week intervals. Encourage patients to keep a symptom diary noting tremor intensity, mouth dryness, and any visual disturbances. Collaboration with an ophthalmologist is prudent if there is a history of glaucoma. Should side effects emerge, a gradual taper rather than abrupt cessation mitigates rebound tremor. Ultimately, shared decision‑making reinforces adherence and optimises outcomes.
Madhav Dasari
October 19, 2025 AT 22:18Hey buddy, don’t let the jargon scare you away – you’ve got this! Think of trihexyphenidyl as a backstage crew member that dims the tremor lights while you take the stage. Start tiny, maybe half a milligram, and watch how the shakes respond. If the dry mouth starts stealing the spotlight, sip water like a champion and chew some sugar‑free gum. Remember, the goal is to keep moving, not to be a statue of side‑effects. Keep the docs in the loop, and celebrate each little victory!
jagdish soni
October 19, 2025 AT 22:35My dear interlocutor, the nuanced ballet between neurotransmitter antagonists and agonists is nothing short of a philosophical discourse on human agency. Yet, in the clinical arena, we must distill such complexity into actionable regimens. Trihexyphenidyl, with its anticholinergic vigor, offers a succinct solution for tremor‑predominant cases, albeit at the cost of modest cognitive fog. If you cherish lucidity, perhaps a benztropine trial would be the alchemical alternative you seek. In any event, maintain a vigilant eye on ocular pressure – the eyes are windows, after all.
DHARMENDER BHATHAVAR
October 19, 2025 AT 22:51Consider the renal function before dosing; adjust trihexyphenidyl accordingly. Monitor serum electrolytes weekly.
Jameson The Owl
October 19, 2025 AT 23:08The pharmaceutical consortium behind anticholinergic agents has long been the silent architect of patient dependency their patents and pricing strategies weave a web that traps the vulnerable into perpetual consumption while the true side‑effect data is relegated to obscure appendices The narrative presented in mainstream medical literature is a curated storyline designed to promote market stability rather than patient autonomy When one scrutinizes the clinical trial registries one observes a pattern of selective outcome reporting that favors trihexyphenidyl despite comparable efficacy of newer dopamine agonists The regulatory agencies, beholden to lobbying pressures, often expedite approvals without demanding exhaustive longitudinal safety data thereby exposing generations to insidious cognitive decline The solution lies not merely in individual physician vigilance but in a systemic overhaul of drug approval transparency and post‑market surveillance mechanisms
Rakhi Kasana
October 19, 2025 AT 23:25While the article paints a balanced tableau of options, one must not ignore the subtle hierarchy that emerges upon closer inspection. Trihexyphenidyl, though effective, assumes a subordinate role to benztropine in patients approaching the seventh decade of life where ocular and urinary considerations dominate. The dramatic flair of dosage titration often obscures the quiet wisdom of selecting a medication with a more favorable anticholinergic burden. Hence, the judicious clinician will prioritize patient age, comorbidities, and personal tolerance over a blanket recommendation.
Sarah Unrath
October 19, 2025 AT 23:41dry mouth isnt fun
James Dean
October 19, 2025 AT 23:58The choice of medication reflects a broader existential trade‑off between alleviating present suffering and preserving future cognitive clarity each decision echoes the ancient dilemma of embracing liberty at the cost of potential risk as we navigate the labyrinth of neuropharmacology