Viral vs. Bacterial Tonsillitis Identifier
Viral Tonsillitis
Typically milder, often accompanied by cold symptoms
Bacterial Tonsillitis
Often severe with high fever and white patches
Select Symptoms Present:
Select symptoms and click "Analyze Symptoms" to determine if the infection is likely viral or bacterial.
When a child develops tonsillitis, parents instantly worry: is it something that will pass on its own or does it need antibiotics? Knowing whether the infection is viral or bacterial guides the right treatment, avoids unnecessary meds, and speeds up recovery.
Quick Takeaways
- Viral tonsillitis usually comes with runny nose, cough, and milder fever.
- Bacterial tonsillitis often shows sudden, high fever, white patches on the tonsils, and swollen lymph nodes.
- Rapid antigen tests and throat cultures are the most reliable ways to confirm a bacterial cause.
- Seek medical care if symptoms last more than 5days, worsen quickly, or affect breathing.
- Supportive home care (hydration, rest, warm fluids) helps both viral and bacterial cases.
Understanding Tonsillitis
Tonsillitis is a inflammation of the palatine tonsils, the two lymph‑rich tissues at the back of the throat. Common attributes include sore throat, difficulty swallowing, and swollen, reddened tonsils. In children, the condition peaks between ages 3 and 7, when the immune system is still learning to fight off germs.
Viral vs. Bacterial Causes
Two main families of germs spark tonsillitis.
Virus is a microscopic infectious agent that replicates inside host cells. Common culprits in children include:
- Rhinovirus (cold virus)
- Influenza A & B
- Parainfluenza
- Epstein‑Barr virus (causes infectious mononucleosis)
These viruses tend to affect the whole upper‑respiratory tract, so symptoms spread beyond the throat.
Bacteria are single‑cell microorganisms that can thrive outside a host. The most frequent bacterial trigger of tonsillitis is Streptococcus pyogenes, the GroupA streptococcus.
Other bacterial agents include:
- Arcanobacterium haemolyticum
- Neisseria gonorrhoeae (rare, usually in adolescents)
Spotting Symptom Differences
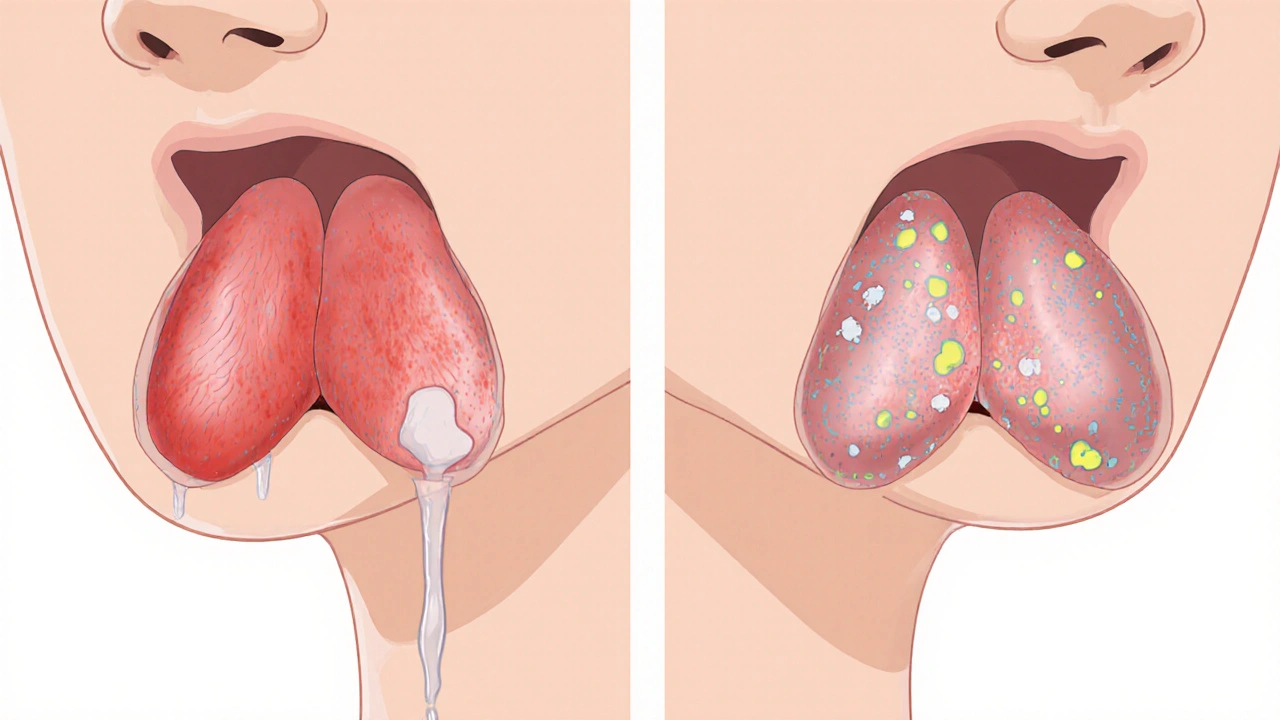
While sore throat is universal, subtle cues point toward a viral or bacterial origin.
| Feature | Viral Tonsillitis | Bacterial Tonsillitis |
|---|---|---|
| Fever | Low‑grade (under 38°C) or intermittent | High (often >39°C) and sudden |
| Throat Appearance | Redness without white spots; may see viral vesicles | White or yellow exudates, pus‑filled patches |
| Neck Lymph Nodes | Soft, mildly tender | Firm, markedly enlarged, tender |
| Associated Cold‑Like Symptoms | Runny nose, cough, sneezing, mild congestion | Usually absent; if present, it’s mild |
| Duration | 5‑7days, then gradual improvement | Often worsens after 2‑3days if untreated |
Remember that symptom overlap is common; a definitive diagnosis often needs a test.
Diagnostic Tools Parents Can Expect
Doctors rely on two quick, office‑based tests.
Rapid antigen test detects specific bacterial proteins (antigens) from a throat swab. Results appear in 10‑15minutes and have about 85% sensitivity for GroupA streptococcus.
If the rapid test is negative but suspicion remains high, a throat culture grows any bacteria present on a specialized medium over 24‑48hours, providing a definitive result.
Blood tests (CBC, ESR, CRP) can highlight an inflammatory response but rarely differentiate viral from bacterial on their own.

When to Seek Medical Care
Not every sore throat warrants a doctor’s visit. Keep an eye out for these red flags:
- Fever above 39°C lasting more than 48hours.
- Severe throat pain that makes drinking fluids impossible.
- Swollen, tender neck nodes that don’t improve.
- Rash, joint pain, or breathing difficulty.
- Symptoms persisting beyond 5days without improvement.
For children under 3years, any sign of tonsillitis should be evaluated promptly, as complications are more common.
Home Care Tips for Both Types
Whether viral or bacterial, supportive care eases discomfort and speeds healing.
- Hydration: Offer water, diluted fruit juice, or ice chips every hour.
- Warm fluids: Chicken broth, herbal teas with honey (for children over 1year), or warm water with a pinch of salt for gargling.
- Humidified air: Use a cool‑mist humidifier in the bedroom.
- Rest: Limit school or daycare attendance once fever subsides.
- Pain relief: Acetaminophen or ibuprofen (dose per weight) can lower fever and soothe throat.
- Avoid aspirin in children due to Reye’s syndrome risk.
- Follow‑up: If a bacterial infection is confirmed, complete the full antibiotic course even if symptoms improve early.
Remember that antibiotics are useless against viruses. Over‑prescribing can lead to resistance and side‑effects, so the test‑guided approach is essential.
Frequently Asked Questions
Can I treat viral tonsillitis at home without seeing a doctor?
If the child’s fever is mild, they can drink fluids, rest, and use over‑the‑counter pain relievers. Watch for worsening symptoms; if they appear, schedule a medical check‑up.
How accurate is the rapid antigen test for strep throat?
The test correctly identifies about 85% of true GroupA strep cases. A negative result doesn’t completely rule out infection, so doctors may send a throat culture if clinical suspicion stays high.
Is it safe to give my child over‑the‑counter antibiotics if I suspect a bacterial infection?
No. Antibiotics should only be taken when a healthcare professional confirms a bacterial cause. Unnecessary use can cause side‑effects and antibiotic resistance.
When will a bacterial tonsillitis start improving after antibiotics?
Most children feel relief within 24‑48hours. Complete the full prescription (usually 10days) to prevent recurrence.
Can tonsillitis lead to complications if left untreated?
Yes. Untreated bacterial infection can cause peritonsillar abscess, rheumatic fever, or kidney inflammation (post‑streptococcal glomerulonephritis). Viral cases rarely lead to serious complications but can trigger secondary bacterial infection.







namrata srivastava
October 8, 2025 AT 13:30When delineating the etiopathogenic dichotomy between virally mediated and bacterially induced tonsillitis, one must invoke a lexicon replete with immunopathological nuance; the cytokine cascade, mucosal immune surveillance, and the stochastic interplay of host genetics coalesce into a clinical tableau that defies superficial appraisal. Moreover, the phenomenological variance in pyrogenic response, exudative morphology, and lymphadenopathic tenacity necessitates a multimodal diagnostic algorithm predicated upon both phenotypic and genotypic parameters. Consequently, reliance solely upon macroscopic inspection is scientifically untenable.
Priyanka arya
October 14, 2025 AT 08:06Yo fam, ever noticed how every time a kid gets a sore throat the “big pharma” machine jumps out with a pen and a prescription like it’s a 🎁? It’s like they’re pulling strings behind the scenes, swapping out natural immunity for a cocktail of meds. 🌐🕵️♀️ Keep your eyes peeled, the truth’s often hidden behind a glossy pamphlet. 🙃💊
Loren Kleinman
October 20, 2025 AT 02:43When a child wakes up with a sore throat, the first thing to notice is how the fever feels. If the temperature is only a little high, it is often a sign that the body is fighting a virus. A high fever that comes on fast usually points to a bacterial infection. Look at the tonsils: if they are covered with white spots, that is a classic clue of bacteria. If the throat is just red and the child has a runny nose, a virus is more likely. The neck nodes can also tell a story; soft and mildly sore nodes go with viruses, while firm, painful nodes are a red flag for bacteria. The duration matters too; a viral illness often gets better after a week, while a bacterial one can get worse after a couple of days. It is important to keep the child hydrated, because fluids help the immune system work. Warm soups and soft drinks can soothe the pain and keep the intake up. Over‑the‑counter pain relievers like acetaminophen can lower the fever safely. If the fever stays high for more than 48 hours, it is wise to see a doctor. A rapid strep test at the clinic can give an answer in minutes. If that test is negative but the doctor still suspects bacteria, a throat culture will be done. The culture takes a day or two but is very accurate. Finally, if a bacterial infection is confirmed, completing the full course of antibiotics is essential, even if the child feels better early on.
Sabrina Goethals
October 25, 2025 AT 21:20i was just thinkin, sooo when your kid’s throat hurts, you gotta watch the fevr, the sore, the runny nose, and ya know, just keep the water flowin, lol. also, don’t forget the honey‑lemon mix for kids over one, it’s like magic, seriously.
Sudha Srinivasan
October 31, 2025 AT 14:56Misusing antibiotics is a negligent act that endangers public health.
Jenny Spurllock
November 6, 2025 AT 09:33Considering the overlap of symptoms, it is prudent to prioritize a test before initiating any antimicrobial therapy, as this safeguards both the child’s recovery trajectory and broader antimicrobial stewardship.
Bart Cheever
November 12, 2025 AT 04:10Honestly, the article throws in a lot of buzzwords but skips the simple truth: if you’re not sure, just ask a doctor and get a swab. Also, the formatting could use better headings.
Maude Rosièere Laqueille
November 17, 2025 AT 22:46Here’s a quick cheat‑sheet for parents: if the fever is under 38°C, the throat is red without patches, and there’s a runny nose, start with fluids, rest, and OTC pain relievers. If you spot white spots, a high fever, or swollen nodes, call your pediatrician for a rapid strep test. Remember, antibiotics are only for confirmed bacterial cases, so don’t self‑prescribe.
Amanda Joseph
November 23, 2025 AT 17:23Wow, because we all needed another lecture on “just call the doctor,” didn’t we? 🙄 Thanks for the groundbreaking insight.
Kevin Aniston
November 29, 2025 AT 12:00I really appreciate the thorough walk‑through, Loren. You broke it down nicely, and your step‑by‑step list is exactly what busy parents need. Keeping hydrated, monitoring fever trends, and knowing when to get a rapid test are solid advice. Thanks for the clarity.
kiran kumar
December 5, 2025 AT 06:36While it’s tempting to see hidden agendas everywhere, the evidence on strep testing is solid and widely validated, so we can trust the standard medical approach without assuming ulterior motives.
Brian Johnson
December 11, 2025 AT 01:13Hydration is key; even mild dehydration can exacerbate throat irritation, so aim for at least half a liter of clear fluids every few hours, especially if the child has a fever.
Jessica Haggard
December 16, 2025 AT 19:50In many cultures, warm turmeric milk is a traditional remedy for sore throats; it’s soothing, has mild anti‑inflammatory properties, and can be a comforting addition alongside modern care.
Alan Clark
December 22, 2025 AT 14:26Stay positive! Most kids bounce back quickly with proper rest and care, and a brief visit to the doctor can clear up any lingering doubts.
Mark Anderson
December 28, 2025 AT 09:03Let’s keep the discussion focused on practical steps and reliable resources, and remember to respect each other’s experiences while sharing useful tips.