Every year, thousands of patients in the U.S. face delays or outright denial of essential medications-not because they can’t afford them, but because there’s simply none left on the shelf. This isn’t a rare glitch. It’s a systemic breakdown. As of April 2025, there are 270 active drug shortages in the United States, and the vast majority are generic drugs. These aren’t niche medications. They’re the backbone of modern care: antibiotics, chemotherapy agents, IV fluids, pain relievers, and heart medications. When they disappear, it doesn’t just inconvenience pharmacies. It puts lives at risk.
Why Do Generic Drugs Keep Running Out?
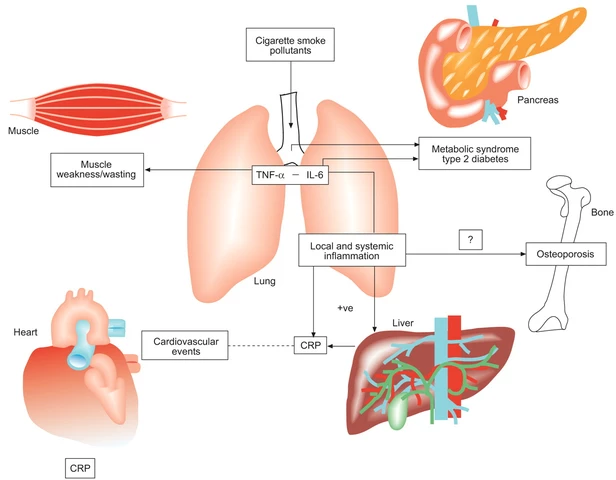
Generic drugs make up 90% of all prescriptions filled in the U.S. But they account for more than 70% of all shortages. Why? The answer isn’t complicated-it’s economic. Most generic drugs sell for pennies. Manufacturers earn gross margins of just 5-10% on sterile injectables, compared to 30-40% for brand-name drugs. When profit margins are this thin, companies don’t invest in backup equipment, extra inventory, or quality upgrades. They run lean. Too lean. Add to that the fact that 70% of these critical drugs have only one or two FDA-approved manufacturers. If one facility shuts down for a quality issue-a common occurrence-there’s no one else to step in. In 2023, the FDA found that 62% of all drug shortages were caused by manufacturing and quality problems. Not lack of demand. Not raw material shortages. Just poor production practices and underinvestment. The global supply chain makes it worse. Over 80% of the active ingredients in U.S. drugs come from just two countries: China and India. These facilities are often far from U.S. regulators, making inspections harder and quality control inconsistent. A single inspection failure in a plant in Hyderabad or Shanghai can ripple across the entire country.Who Gets Hurt the Most?
It’s not just patients who wait. It’s the people who need treatment right now. Oncology departments are among the hardest hit. Cisplatin, a chemotherapy drug used for lung, ovarian, and testicular cancers, has been in short supply for over two years. Hospitals have had to switch to less effective alternatives or delay treatments. A 2024 survey found that 67% of cancer centers modified chemotherapy regimens because of shortages. In hospitals, vancomycin-used to treat deadly bacterial infections like MRSA-has been unavailable for months. Pharmacists are forced to use more expensive, less proven drugs. One hospital pharmacist in Texas told a Reddit community: “We’ve been out of vancomycin powder for reconstitution for 8 months now. Patients are getting alternatives that are less effective and more toxic.” Even chronic pain patients aren’t safe. When opioid generics like oxycodone or hydrocodone run out, patients with legitimate medical needs are denied refills. Emergency rooms see a spike in uncontrolled pain cases. Independent pharmacies report that 43% of patients abandon prescriptions altogether because they can’t get the drug or can’t afford the substitute.
The Hidden Cost to Healthcare Systems
Shortages don’t just hurt patients-they overload the system. Pharmacists now spend 15-20 hours a week just managing shortages. That’s not time spent counseling patients or reviewing medication safety. It’s time spent calling other pharmacies, checking alternate suppliers, updating electronic records, and reprogramming automated dispensing machines. Hospitals have to buy substitute drugs at inflated prices. A 2024 report from the HHS Office of Planning and Evaluation found that generic drugs in shortage saw price increases of 14.6% on average. But the alternatives? Sometimes they cost three times as much. The American Hospital Association estimates U.S. hospitals spend $213 million annually just to cope with drug shortages. That’s money that could go toward hiring nurses, upgrading equipment, or expanding mental health services. And it’s getting worse. The number of FDA-registered generic drug manufacturing facilities in the U.S. dropped by 22% between 2015 and 2024. Meanwhile, the top 10 generic manufacturers now control 60% of the market-up from 45% a decade ago. Less competition. Less redundancy. More risk.Why Sterile Injectables Are the Weakest Link
Not all generic drugs are equally vulnerable. Sterile injectables-drugs given through IV or injection-are the most likely to be in short supply. Why? They require clean rooms, specialized equipment, and highly trained staff. A single contamination can shut down a whole production line. These drugs are also low-margin, high-volume products. Manufacturers don’t want to spend millions on redundant lines for a drug that sells for $2 a vial. In 2025, over 60% of all drug shortages were sterile injectables. That includes saline bags, antibiotics like ampicillin, and critical drugs like epinephrine and insulin. When these run out, hospitals can’t perform surgeries, treat sepsis, or stabilize heart attack patients.






Georgia Brach
December 22, 2025 AT 20:10The data here is meticulously compiled, but it ignores the fundamental truth: the market doesn't fail because of greed-it fails because regulation is a theater of compliance. The FDA approves facilities that shouldn't be allowed to produce saline, then wonders why shortages persist. This isn't a supply chain issue. It's a regulatory capture issue.
Payson Mattes
December 23, 2025 AT 13:01Okay but have you heard about the secret Chinese lab in Guangdong that’s been flooding the US with fake insulin? I know a guy whose cousin works at the FDA and he says they’ve known since 2021 but they’re covering it up because of trade deals. Also, the WHO is in on it. They’re all linked to Big Pharma. You think these shortages are accidental? Nah. It’s a ploy to push people toward expensive biologics. Wake up.
siddharth tiwari
December 24, 2025 AT 22:44in india we dont have this problem cause we make our own generics. why do u rely on china and india for drugs when u have so many pharma companies? u just want cheap cheap cheap. then cry when it breaks. its not rocket science. stop blaming others. fix ur own system.
Diana Alime
December 25, 2025 AT 16:59so like… i had to wait 3 weeks for my dad’s chemo drug last year. they gave us some weird substitute that made him throw up for 48 hours straight. my mom had to call 17 pharmacies. i swear i cried in the parking lot of CVS. why is this even a thing? we’re the richest country on earth and we can’t keep antibiotics in stock? someone’s getting rich off this. and it’s not us.
Adarsh Dubey
December 27, 2025 AT 12:53There’s a quiet irony here: the same market logic that makes generics affordable also makes them fragile. A system optimized for efficiency becomes brittle under stress. The solution isn’t necessarily more regulation-it’s redefining value. What if we paid for reliability, not just price? It’s not anti-capitalist. It’s pragmatic capitalism.
Bartholomew Henry Allen
December 27, 2025 AT 17:41Foreign factories foreign regulators foreign profits American patients suffer. This is what happens when you outsource your medicine. We used to make our own. We had the plants. We had the workers. Now we beg for vials like beggars. Fix the supply chain or shut the borders. Either way stop pretending this is a technical problem.
Jeffrey Frye
December 28, 2025 AT 23:20you know what’s wild? the fact that the same companies that make these cheap generics are the ones lobbying against price controls. they’re not poor little victims. they’re the ones who chose to underinvest. then they get surprised when a single batch of contaminated saline takes down the whole system. it’s not a mystery. it’s math.
niharika hardikar
December 29, 2025 AT 05:58The structural inefficiencies in the generic pharmaceutical supply chain are exacerbated by a lack of horizontal integration and vertical coordination. The absence of buffer inventory mechanisms, coupled with monopsonistic procurement practices by PBMs, creates systemic vulnerability. The FDA’s current risk mitigation protocols are reactive rather than anticipatory, failing to incorporate real-time predictive analytics derived from global manufacturing telemetry.
Jillian Angus
December 30, 2025 AT 07:25my pharmacist just shrugged when i asked about my blood pressure med. said 'we got it next week maybe' like it was a delayed pizza. i just nodded. what else can you do? i guess i’ll keep taking half doses until the universe decides to fix this
Aurora Daisy
December 31, 2025 AT 10:36Oh look, the Americans are shocked that their healthcare system is a dumpster fire. You outsource your manufacturing, deregulate your monopolies, and then act surprised when people can’t get antibiotics. Meanwhile, the NHS just orders from a dozen suppliers and calls it a day. Maybe stop treating medicine like a stock market ticker and more like… life support?
Paula Villete
January 1, 2026 AT 21:38They say the market rewards efficiency. But efficiency without resilience is just fragility with a business plan. We don’t need more regulations-we need a new metric. What if we rated drug manufacturers not on cost per vial, but on continuity of supply? On redundancy? On ethical labor? Maybe then we’d stop pretending this is about economics. It’s about ethics. And we’ve been failing that test for decades.