When your breathing gets worse than usual-when you can’t catch your breath even sitting still, your cough turns harsher, and your mucus turns thick and green-you’re not just having a bad day. You’re having a COPD exacerbation. These flare-ups don’t come out of nowhere. They’re a dangerous signal that your lungs are under attack, and if you ignore them, they can land you in the hospital-or worse.
What Exactly Is a COPD Exacerbation?
A COPD exacerbation is when your chronic obstructive pulmonary disease suddenly gets much worse. It’s not just more coughing or a little more shortness of breath. It’s a sharp drop in lung function that lasts for days, sometimes weeks. Your airways swell, mucus builds up, and your body struggles to get enough oxygen. This isn’t normal fluctuation. This is a medical event that needs attention.Think of your lungs like a pair of old, worn-out bellows. COPD has already made them stiff and clogged. Now, something-like a cold virus or polluted air-forces them to work harder. The result? You feel like you’re breathing through a straw. Studies show that over 75% of these flare-ups are caused by infections. The rest? Triggers like smoke, cold air, or chemical fumes.
Each time this happens, your lungs don’t fully recover. Even after symptoms fade, you may lose a little more lung function forever. That’s why every exacerbation matters. The more you have, the faster your condition declines. People with advanced COPD can have up to three flare-ups a year. And each one raises the risk of hospitalization, heart problems, and death.
Top Triggers of COPD Flare-Ups
Not all exacerbations look the same, but they almost always start with the same culprits.Infections are the biggest enemy. Viruses like the common cold, flu, and RSV cause about half of all flare-ups. Bacteria like Haemophilus influenzae, Streptococcus pneumoniae, and Moraxella catarrhalis are responsible for another quarter. Even COVID-19 can trigger an exacerbation, though recent data shows inhaled COPD medications may help reduce its severity.
Environmental irritants are just as dangerous. Smoke-whether from cigarettes, fireplaces, or wildfires-is a major trigger. So is air pollution. Even strong smells like perfume, cleaning products, or paint fumes can set off a flare-up. Cold, dry air makes your airways tighten up. If you go outside without covering your nose and mouth in winter, you’re putting yourself at risk.
Some triggers are harder to spot. Stress, poor sleep, skipping your daily inhaler, or even changes in weather pressure can make things worse. It’s not always one big event. Sometimes, it’s a combination of small things piling up.
How to Spot a Flare-Up Early
The key to surviving a COPD exacerbation is catching it early. Don’t wait until you’re gasping for air. Learn your baseline-what your breathing, cough, and mucus look like on a good day. Then watch for these warning signs:- More coughing than usual, especially if it’s worse at night
- Mucus that’s thicker, darker (yellow, green, or bloody), or more than normal
- Shortness of breath during simple tasks like walking to the bathroom
- Wheezing or a tight feeling in your chest
- Feeling more tired than normal, even after resting
- Fever, chills, or body aches-signs your body is fighting an infection
- Difficulty sleeping because you can’t breathe
If two or more of these symptoms last for more than two days, you’re likely having an exacerbation. Don’t assume it’ll pass. That’s when you act.

Emergency Symptoms: When to Call 911
Some flare-ups turn life-threatening fast. If you have any of these, get help immediately:- Blue lips or fingernails (a sign of low oxygen)
- Confusion, dizziness, or extreme sleepiness
- Heart rate over 100 beats per minute without exertion
- Severe difficulty speaking in full sentences
- Using neck or stomach muscles to breathe
These aren’t signs to wait on. Low oxygen levels can damage your heart and brain in minutes. If you’re using your rescue inhaler and it’s not helping, or if you feel like you’re suffocating, call emergency services right away.
What Happens in the ER
When you arrive at the hospital with a severe COPD exacerbation, the team moves fast. Their first goal? Get oxygen into your blood. They’ll check your oxygen levels with a pulse oximeter and may give you extra oxygen through a mask or nasal prongs. Too much oxygen can be dangerous for some COPD patients, so they’ll monitor it closely.Next, they’ll look for infection. A chest X-ray, blood tests, and sometimes a sputum sample help them decide if you need antibiotics. Most people get a short course of oral steroids-like prednisone-to reduce airway swelling. Inhaled bronchodilators are given through a nebulizer to open your airways quickly.
If your breathing doesn’t improve, you might need non-invasive ventilation (NIV) with a mask that pushes air into your lungs. In rare cases, a breathing tube is inserted. Hospital stays average 5 to 7 days, but recovery can take weeks. And even after you leave, your lungs may never fully return to how they were before the flare-up.

Home Treatment: What You Can Do
Not every flare-up needs the ER. If symptoms are mild to moderate, follow your COPD Action Plan. Most doctors give patients a personalized plan that includes:- Increasing your rescue inhaler (like albuterol) as directed-usually every 4 to 6 hours
- Starting oral steroids (like prednisone) for 5 to 14 days
- Using antibiotics if your mucus changes color or you have a fever
- Staying hydrated to thin mucus
- Resting and avoiding triggers
Don’t guess. Stick to your plan. If symptoms don’t improve in 48 hours, call your doctor. If they get worse, go to the ER. Delaying treatment increases your risk of complications and longer recovery.
Prevention: Your Best Defense
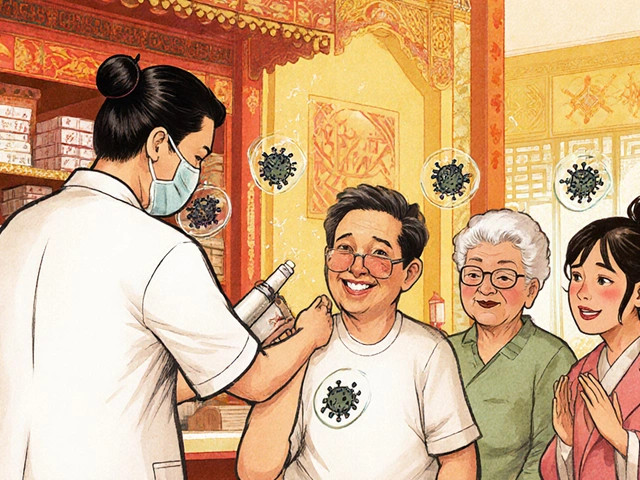
The best way to avoid exacerbations is to stop them before they start.- Get vaccinated. Annual flu shots and pneumococcal vaccines (PCV15 or PCV20) cut infection-related flare-ups by up to 50%.
- Take your daily meds. Inhaled corticosteroids and long-acting bronchodilators keep your airways open and reduce inflammation. Skipping them-even for a day-raises your risk.
- Avoid smoke and fumes. Quit smoking if you haven’t. Stay away from secondhand smoke, fireplaces, and strong chemicals. Use air purifiers indoors.
- Wash your hands. Frequent handwashing and avoiding sick people during cold and flu season can prevent half of all infections.
- Monitor your symptoms daily. Keep a simple log: How’s your breathing? Any change in mucus? This helps you spot trends before they become emergencies.
Recent studies show that consistent use of inhaled COPD medications may even protect against severe outcomes from viruses like COVID-19. It’s not a guarantee, but it’s one more reason to stay on your treatment plan.
The Bigger Picture
COPD exacerbations aren’t just about lungs. They trigger systemic inflammation-meaning your whole body is under stress. That’s why people who have frequent flare-ups are more likely to have heart attacks, strokes, or blood clots. Each exacerbation is a warning sign that your body is struggling.More than 10 million doctor visits in the U.S. each year are due to COPD flare-ups. That’s not just a health issue-it’s a financial and emotional burden on families and the healthcare system. But the good news? Most of these events are preventable.
Knowing your triggers, recognizing the early signs, and acting fast can keep you out of the hospital and preserve your lung function. It’s not about being perfect. It’s about being aware. Because when your breathing fails, there’s no time to learn what to do. You have to know already.
How long does a COPD exacerbation last?
Most COPD flare-ups last 7 to 14 days, but some can stretch for weeks. Even after symptoms improve, lung function may not return to its pre-flare-up level for up to 8 weeks. Each episode can cause permanent damage, which is why early treatment matters.
Can COPD exacerbations be prevented?
Yes, many can. The most effective strategies include getting annual flu and pneumonia vaccines, taking daily prescribed medications, avoiding smoke and pollution, washing hands frequently, and following a personalized action plan. People who stick to their treatment plan have up to 50% fewer flare-ups.
What’s the difference between a COPD flare-up and a cold?
A cold usually causes mild symptoms like a runny nose and sore throat that improve in a few days. A COPD flare-up involves worsening breathing, increased mucus (especially if it’s thick or colored), and symptoms lasting more than two days. If your breathing gets worse-not just your nose-it’s likely a flare-up, not just a cold.
Should I go to the ER if my rescue inhaler doesn’t help?
Yes. If your rescue inhaler (like albuterol) doesn’t relieve your symptoms within 20-30 minutes, or if you’re using it more than every 4 hours, you need emergency care. This means your airways are severely blocked and you may be running out of oxygen.
Does oxygen therapy help during a COPD exacerbation?
Yes, but it must be carefully controlled. Low oxygen levels are dangerous and need correction. However, too much oxygen can suppress breathing in some COPD patients. Emergency teams use pulse oximeters to give just enough oxygen to keep levels above 88-92%. Never adjust oxygen at home without medical advice.






Jay Ara
December 26, 2025 AT 00:52man i been there so many times
one day i just felt like my chest was full of concrete
took my inhaler nothin
called my wife she drove me straight to er
they gave me steroids and oxygen
stayed 5 days
learned the hard way dont wait
Michael Bond
December 26, 2025 AT 22:13Get the flu shot. Every year. No excuses.
christian ebongue
December 27, 2025 AT 08:11oh so now its my fault my lungs are garbage because i skipped my inhaler for 2 days
thanks for the guilt trip doc
david jackson
December 28, 2025 AT 07:18you know what really gets me about these exacerbations
its not just the gasping
its the silence
the way your own body betrays you
you used to hike mountains
now you cant tie your shoes without stopping
and the worst part
no one sees it
you look fine
you smile
you say im okay
but inside your lungs are screaming
and the world just keeps spinning
like your suffering is background noise
and every flare-up
is just another brick in the wall
that slowly buries you alive
and nobody notices until you stop breathing
Jody Kennedy
December 28, 2025 AT 19:29you got this
every breath you take right now
is a victory
and if you need to call someone
call me
i’ll sit on the phone with you
until you feel better
josue robert figueroa salazar
December 29, 2025 AT 02:48so let me get this straight
if i get sick
and my lungs give out
its because i didnt wash my hands enough
and didnt take my meds
and didnt avoid every single smell in the universe
but when rich people get cancer
its genetics
when poor people get COPD
its personal failure
real deep
Sarah Holmes
December 30, 2025 AT 15:57It is not merely a medical condition; it is a metaphysical confrontation with mortality, wherein the very act of respiration becomes an existential burden. One cannot help but observe the tragic irony: that the most fundamental of human functions-drawing air into the lungs-is now a battlefield, a site of systemic collapse. The pharmaceutical interventions, while palliative, are but Band-Aids on a hemorrhaging soul. The vaccines? A temporal reprieve. The action plans? A bureaucratic illusion of control. In the end, the body is a vessel of decay, and we are all merely tenants awaiting eviction. One must ask: is it not more dignified to surrender gracefully than to endure this slow, suffocating audit of one’s own fragility?
carissa projo
December 31, 2025 AT 16:37you know what i see in all of this
its not just about lungs
its about how we treat people who struggle silently
we hand out checklists like they’re magic spells
but we forget to sit with them
when they’re too tired to hold the inhaler
when they’re scared to call for help
when they feel like a burden
i’ve watched my neighbor
she’s got the plan
she’s got the meds
but she’s alone
and loneliness
is the quietest trigger of all
so if you’re reading this
check on someone
not to fix them
but to say
i see you
and you’re not alone
even on the days
when breathing feels like climbing a mountain